Revolutionary Crispr Gene Editing Speeds from Lab to Treatment Room
Just a decade after Crispr was invented, the first drug to make use of the revolutionary gene-editing technology will be with regulators by the end of the year, with the promise that it will eventually transform the treatment of genetic diseases.
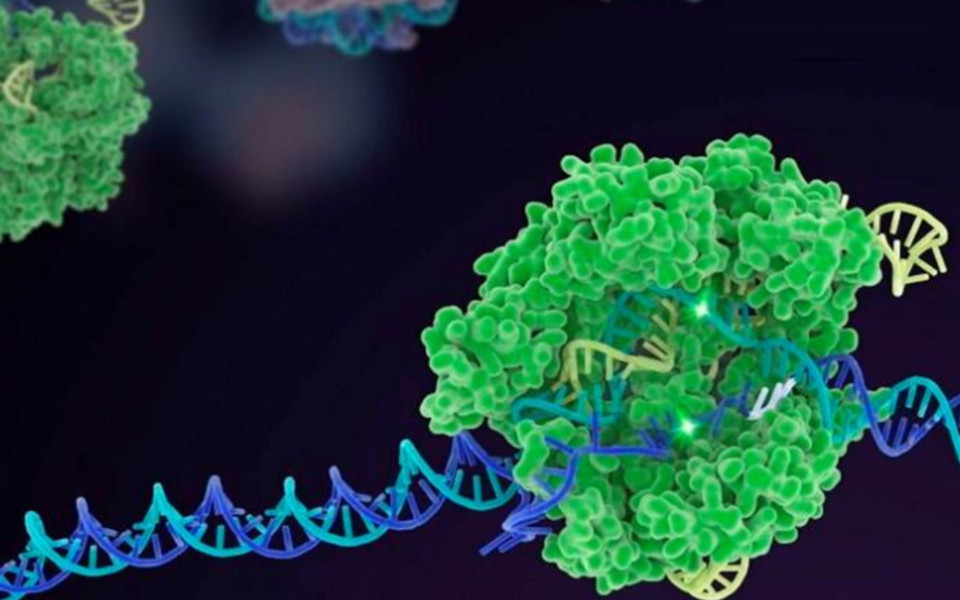
In 2012, Nobel Prize winners Jennifer Doudna and Emmanuelle Charpentier published a scientific paper proving a key part of the bacterial immune system could be used to cut DNA: disrupting, deleting or correcting genetic errors.
Their discovery started a race by start-ups to create transformative — and possibly even curative — treatments, which has developed much faster than previous advances in biology.
The first to close in on success is Crispr Therapeutics which, in partnership with biotech group Vertex, expects to submit late stage trial data seeking approval for its treatment for the inherited blood diseases sickle cell anaemia and beta thalassaemia to EU and UK regulators at the end of 2022.
Its latest data show all sickle cell patients were free of symptoms and that the vast majority of beta thalassaemia patients were no longer reliant on transfusions.
Doudna said it was “extraordinary” that sickle cell patients such as Victoria Gray, who was treated in the first trial three years ago, have already been “effectively cured of genetic disease”.
“One of the most surprising and exciting things to me is just how rapidly it’s been possible to apply it in the clinic,” she told the Financial Times. “It has been the foundation for multiple companies created tens of billions of dollars in value and foundation for multiple companies, created tens of billions of dollars in value, and many, many thousands of jobs.”
Accordingly, big pharma groups like Pfizer, Bayer, and Regeneron have taken note, forming partnerships with the pioneers. Analysts predict drugmakers will soon be in the market to buy Crispr companies, partly in the hope of acquiring the tool to improve innovative treatments for cancer.
But the development of Crispr also raised significant questions about the ethics of gene editing and its long-term effects.
Many scientists condemned a Chinese researcher who revealed in 2018 that he had edited the genetic code of recently born twin girls . There have also been intellectual property lawsuits, debating the relative contributions of Doudna and Charpentier, andthe Broad Institute’s Feng Zhang, who wrote a paper showing how Crispr works in humans.
For the start-ups working on Crispr drugs, the general slump in biotech stocks, some failed trials and safety concerns in the adjacent field of gene therapy, have made life more difficult. It has become harder to convince investors that this revolution has staying power.
And when the first Crispr drugs are approved, there is the question of persuading insurers and governments to pay the high price tags, just as drug pricing reform is back on the agenda in the US, the world’s largest pharmaceutical market.
Biotech’s “transistor” moment
Vijay Pande, a general partner at venture capital firm Andreessen Horowitz, compares Crispr to the invention of the transistor, which revolutionized computer design.
“We are just at the very earliest stages. I think where we are now is maybe akin to the1960s in computers,” he said. The biggest remaining scientific challenge is delivering Crispr to other organs, beyond the relatively easier areas of the blood, liver and eyes. Kiran Musunuru, a gene editing specialist at the University of Pennsylvania, said researchers are already starting to make some progress. “It’itblitht10”hid“Tht’itbtfti “It’s going to blow up in the next 10 years,” he said.
“That’s going to be transformative because it is going to greatly expand the number of diseases that we can treat with Crispr in patients.” Crispr’s scientific success is partly because it can use or adapt technology developed and applied in gene therapy, a method of delivering missing genes to patients that has been used to treat life-threatening conditions like spinal muscular atrophy.
It has also benefited from the explosion of data on the human genome, which helps scientists understand which genes to target.
“The thing about Crispr that’s so remarkable is that the timing was right,” Doudna said. Scientists quickly built on the original discovery. About five years ago, they created base editing, which can make more precise changes. Pfizer has partnered with base editing company Beam Therapeutics in a deal worth up to $1.35 bn, hoping to deploy its expertise in lipid nanoparticles, developed from its work on the Covid-19 vaccine, as a way of delivering Crispr treatments.
While most trials are still targeting rare diseases, base-editing company Verve recently treated its first patient in a study targeting a genetic condition that causes high cholesterol, which could one day be used in a market of millions of patients.
Crispr is also being used to enhance a type of individually tailored cancer treatment called CAR-T therapy, which could be what tempts pharmaceutical companies into acquiring smaller specialist biotechs, according to Jefferies analyst Maury Raycroft.
Big pharma groups are sitting on huge cash piles and a number of them need to buildup their drug pipelines before significant patent expiries at the end of the decade.
John Leonard, chief executive of Intellia, which did the first in-body Crispr delivery (rather than removing cells, modifying and returning them) as part of its trial for a liver disease treatment, said it is “essentially a foregone conclusion” that every large pharmaceutical company will have to have some Crispr capability.